
Online Claims Filing Convenience
With your ArmadaCare plan, you have access to both a Member Portal and mobile app. Let’s review what you can do on each platform.

Getting Started: First-Time User
To get started, access your Member Portal at armadacare.com/myaccount. Click the “Get Started” button in the “First-Time User” box on your Member Portal login page. Once your account is created, you will be able to:
- Use your Username and Password to log in on the Member Portal as an Existing User. (Don’t forget to bookmark your Member Portal on your web browser.)
- Download and sign into the mobile app.
Steps to Take to File a Claim
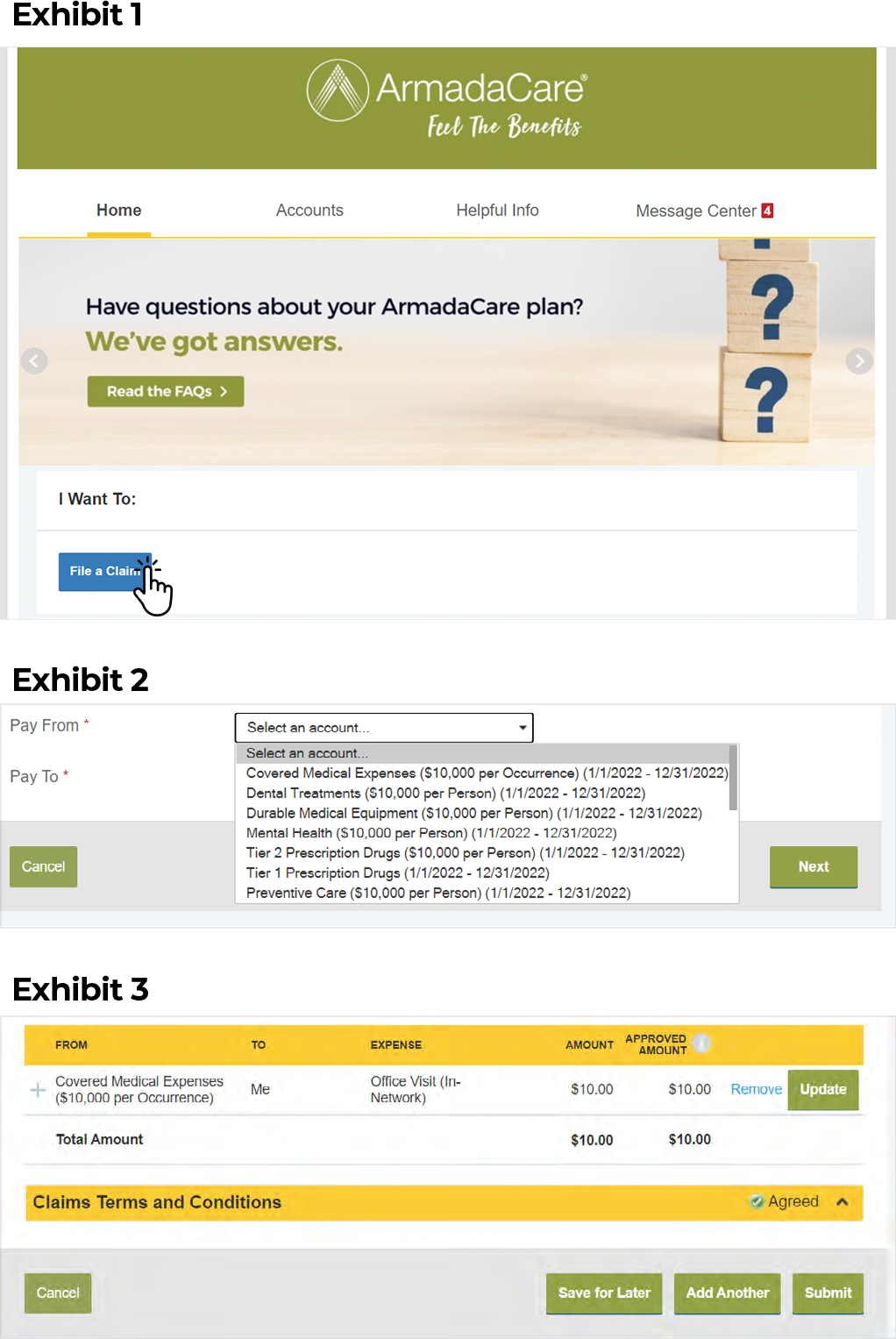
- On the Home Page, select the “I Want To… File A Claim” button. (Exhibit 1)
- Scroll down to the Pay From dropdown menu and click on the down arrow to select the account type. (Exhibit 2)
- Then select Me from the Pay To dropdown menu. Click Next.
- Click on Upload Valid Documentation and follow the onscreen prompts to upload the required documentation, i.e., Explanation of Benefits (EOB), provider invoice or a detailed receipt. Documentation requirements vary for each claim type. Max upload is 4 documents. Once complete, click Next.
- Complete the Claim Details section and select Next to proceed. If you are submitting more than one claim, click Add Another on the next screen.
- When all claims are entered, agree to the Terms and Conditions, and click Submit to send the claims for processing. (Exhibit 3)
Note: Filing multiple claims? Use Submit and not the “save for later” button. Once you log out, your claims will be deleted if they are not submitted.
How To View Notifications
- On the Home Page, look under the Tasks section to see notifications in blue for claims that require action, such as providing missing claim documentation.
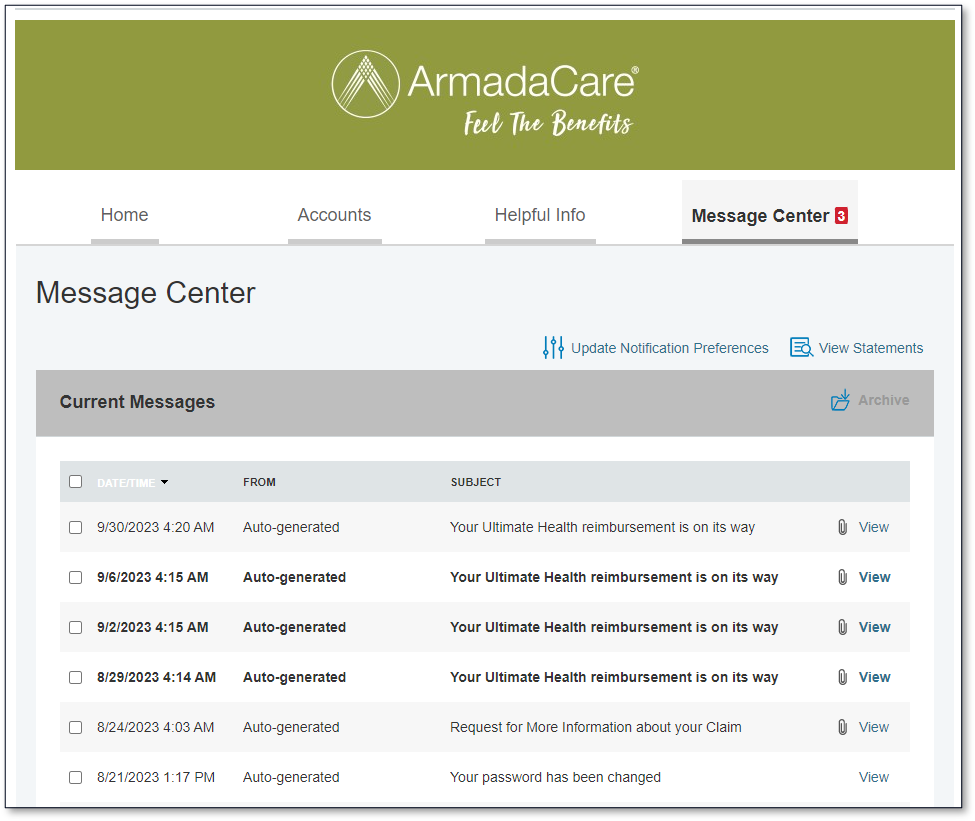
- By clicking on the Message Center tab in the top right, you can view all notifications, including Denials, Requests for More Information and Payment Notifications in more detail. Access your notifications by clicking View and then the attachment name. Only rows with a paperclip icon will have an attachment to view.
Note: If the Message Center attachments aren’t visible, you’ll need to disable your web browser pop-up blocker or add your Member Portal to the list of those allowed to show pop-ups within your web browser. Take these steps to disable pop-up blockers in the most common internet browsers.
How to: Upload Documentation to an Existing Claim
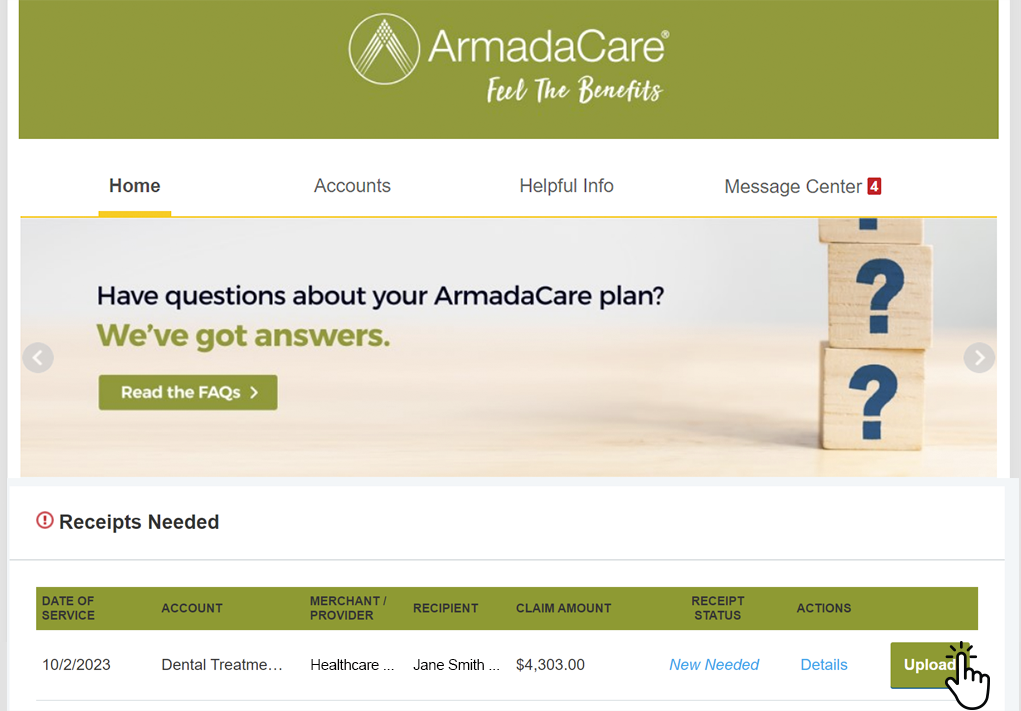
Your claim won’t be processed unless it has the proper documentation. If you receive a Request for More Information (RMI) on a claim, you don’t need to submit a whole new claim with that paperwork. Simply add the missing documentation to that claim following these steps:
- On the Home page of your online Member Portal, scroll down to the Tasks.
- Click on Receipts Needed to view your claims.
- Click on Details and Review Request(s) to view the documentation required to process the claim.
- Click on Upload to upload additional documentation. Choose the file you want to add (from your computer) and click Submit.
- The claim will go back in queue for processing, which typically takes 5-7 business days.

Seeing Double?
For 3 months of the year, you will see twice as many benefit categories for claim filing: one set is for the current plan year and the other set is for the prior plan year. Once your ArmadaCare plan renews, you have 90 days to file claims for the prior plan year. Be sure to look at the plan year in parentheses and file your claims accordingly. Learn more here.
ArmadaCare's Mobile App
Take a quick tour on how to use the mobile app by watching this video.
- Download the Mobile App by searching for ArmadaCare in your device’s app store.
- Use your same username and password as the Member Portal to log in to the mobile app.
- Next, you will be asked to assign a four-digit passcode. You can then choose to activate Face ID or Touch ID for ease in logging in next time.
FAQs
Still have questions? Contact the Member Services team Monday-Friday 8:30 a.m. to 8:00 p.m. Eastern by calling 1-888-895-0196 or emailing support@armadacare.com. If you would prefer to schedule time to talk, click here.
Exhibits and member portal images are for visual only. Plan names and benefit categories may be different than your ArmadaCare plan.


